Uveitis, in itself, isn’t necessarily the cause of blindness in patients. As with many other diseases, it’s not the disease itself that creates the most damage, but the complications and ancillary issues, which are often related and tend to snowball.
“Noninfectious intermediate uveitis, posterior uveitis, or panuveitis, particularly persistent disease, is associated with a substantial risk of ocular complications” (Dick, Andrew D., et al., 2016).
Some conditions are brought on due to the eye being in a constant state of inflammation or just being “messed with” too much (multiple surgeries, shots, etc). Treatments for uveitis, steroids, in particular, have side effects that tend to create complications for the eye that then also must be treated.
I’ve listed the main complications that I’ve encountered (except for retinal detachment, fingers crossed).
Cataracts
A cataract forms when the proteins in the eye start to break down and clump together causing a clouding of the eye. Light is not able to enter through this cloud and eventual vision degrades. Cataracts can be brought on by ocular surgery or prolonged use of high doses of steroids.

Symptoms: Clouded, blurred, or dim vision
Treatment: During cataract surgery, the lens is removed and replaced by an artificial lens made specifically for the patient’s eye. For patients with eye disease, a multifocal lens may not be an option, so the patient will have to choose a near-sided or far-sided lens. There is a risk of developing a secondary cataract after the surgery
More info: Cataracts * Cataract surgery in patients with history of uveitis (2012)
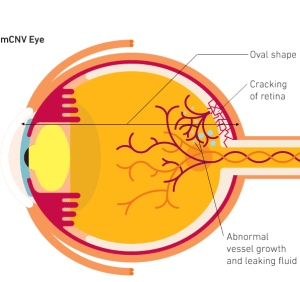
Choroidal Neovascularization & Subretinal Fibrosis
Choroidal neovascularization (CNV) is the growth of new, damaging blood vessels beneath the retina. These blood vessels grow in the choroid and break through the barrier between the choroid and the retina. When they leak in the retina they cause vision loss.
Symptoms: Distorted vision, change in color vision, or loss of vision without pain are symptoms of choroidal neovascularization.
Treatment: Intravitreal anti-VEGF therapy such as Avastin is most common. Laser photocoagulation (using a laser to shrink or destroy the abnormal blood vessels), immunosuppressive, and photodynamic therapy (PDT) are also treatments.
More Info: What is Choroidal Neovascularization? * Inflammatory Choroidal Neovascular Membranes in Patients With Noninfectious Uveitis: The Place of Intravitreal Anti-VEGF Therapy (2020) * Photodynamic therapy: current role in the treatment of chorioretinal conditions (2016) * Related Blog post: The latest on my uveitis
Subretinal fibrosis is the development of scarring (of either band-like or plaque-like areas of fibrosis) underneath the retina due to choroidal neovascularization (CNV).
Treatment: None currently developed.
More info: [Because CNV is common in patients with Age-related Macular Degeneration (AMD), many studies related to subretinal fibrosis are related to AMD.] Choroidal pericytes promote subretinal fibrosis after experimental photocoagulation (2018) * Molecular mechanisms of subretinal fibrosis in age-related macular degeneration (2015)
Epiretinal Membrane
An Epiretinal Membrane (ERM) is a condition where a very thin layer of scar tissue forms on the surface of the retina.
Symptoms: Often no symptoms, decreased vision (particularly central vision), blurred or distorted vision, double vision
Treatment: Vitrectomy (replacement of vitreous gel filling inside of the eye with saline or gas)
More Info: Epiretinal Membranes
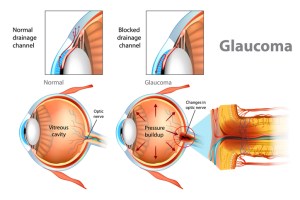
High Intraocular Pressure / “Steroid Induced Glaucoma”
Normal interocular pressure (IOP) ranges from 12-21 mmHg. Long-term and/or high dosage steroid usage for the treatment of uveitis often leads to elevated IOP, or “steroid-induced glaucoma“. It seems the trabecular meshwork of the eye that allows for fluid to flow out of the eye gets plugged up through a variety of mechanisms. Fluid builds up around the front of the eye; this increases eye pressure which can damage the optic nerve. Damage to the optic nerve is irreversible. According to the Standardization of Uveitis Nomenclature Working Group, the threshold for considering a rise in interocular pressure due to corticosteroid to be substantial is 10 mmHg or greater.
Symptoms: Blurred vision, eye pain, and headaches. High IOP/glaucoma can have no symptoms, which is why pressure checks are important while being treated with steroid medications.
Treatment:
- Eye Drops: Eye drops may be prescribed to attempt to reduce the IOP by decreasing the production of intraocular fluid, such as:
- Combigan (brimonidine and timolol)
- Azopt (brinzolamide)
- Oral Medication: There are oral medications that essentially do the same thing as the drops, such as:
- Selective Laser Trabeculopasty (SLT): Selective Laser Trabeculoplasty is an in-office procedure during with the doctor uses a laser to stimulate the trabecular meshwork to improve drainage. Improvement may last from 3-5 years and the procedure can be repeated. This is an option for those who have difficulty with drops.
- Trabeculectomy: A Trabeculectomy is a procedure that lowers the pressure in the eye by removing a piece of the trabecular meshwork to allow for drainage but still in a controlled manner. The fluid drains through a piece of tissue stitched on the eye to a bleb (small blister or reservoir) just under the eye surface. This is a procedure that is done in an operating room under local anesthesia and takes up to six weeks for recovery, depending on the patient. Complications can include scarring of the bleb, especially in younger patients, and anti-scarring drops are often prescribed. Cataract formation is often a side effect of this procedure; cataract surgery is sometimes preformed at the same time but can be preformed at a later date.
- Aqueous Shunt Implantation: This procedure is often done in conjunction with a trabeculectomy or after a trabeculectomy alone has failed to lower pressure in a patient. A device (a tiny silicone shunt or tube) is inserted in the hole created by the trabeculectomy to ensure the hole does not scar over. The shunt and end plate are covered with a piece of donor eye tissue.
- Ahmed Glaucoma Valve: The Ahmed Glaucoma Valve contains a type of valve that helps to prevent very low eye pressure during the first few weeks after surgery.
- Baerveldt Glaucoma Implant and Molteno Glacoma Implant: The Baerveldt and Molteno implants have no valve and must be blocked with a stitch at the time of surgery to prevent the shunt from excessive draining in the first few weeks after surgery (which would cause the eye pressure to drop too low).
More info: Glaucoma.org * Steroid-induced Glaucoma: An Avoidable Irreversible Blindness (2017)
Macular Edema
Macular Edema is a fluid buildup in the macula (center of the retina) that causes it to swell and thicken which distorts vision.

Symptoms: Typically macular edema is painless and the first signs will be blurred or washed out vision.
Treatment: Treatment typically includes Anti-Vegf Injections, steroids (via injection or drops), or laser treatment.
More Info: What is Macular Edema? * Therapy applied directly inside the eye best for treating uveitic macular edema (2018)
Papillitis
Papillitis, also known as optic neuritis, is characterized by inflammation and deterioration of the portion of the optic nerve known as the optic papilla (the part where the optic nerve enters the eye, i.e. the normal “blind spot”). Loss of vision can occur within a few hours of onset.

Symptoms: Loss of vision, changes in color vision, and eye pain
Treatment: Corticosteroids
More Info: Inflammatory Papillitis in Uveitis: Response to Treatment and Use of Optic Nerve Optical Coherence Tomography for Monitoring (2014-abstract)
Pitosis
Ptosis is the drooping of the upper eyelid. This can occur after surgical procedures involving the eye.

Symptoms: Droopy eyelid
Treatment: Blepharoplasty (eyelid surgery) or Upneeq (drops)
More Info: Ptosis: Droopy eyelids
Retinal Detachment
Retinal detachment is when the retina pulls away from the layer of blood vessels it is typically attached to. Retinal detachment is very serious and can quickly result in permanent vision loss. Exudative retinal detachment occurs when fluid accumulates beneath the retina and is the type of detachment most associated with uveitis and/or ocular surgery.
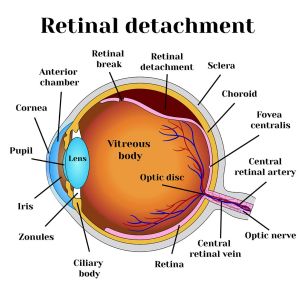
Symptoms: Appearance of floaters, sudden flashes of light, or a shadow in the visual field are symptoms of retinal detachment, particularly if recovering from surgery.
Treatment:
- Pneumatic Retinopexy and Scleral Buckle: Procedures for repairing retina tears depend of the severity of the tear. During pneumatic retinopexy, a gas bubble is injected into the eye. The bubble presses against the detached retina and pushes it back into place. A laser is used to reattach the retina (cryotherapy). scleral buckle may be performed. During a scleral buckle, a flexible band is placed around the eye to counteract the force that is pulling the retina out of place. The fluid behind the detached retina will be drained, and the retina should return to its normal position.
- Vitrectomy: A vitrectomy is the most common procedure for complex retinal detachment, particularly the exudative sort that is not caused by a tear.
More information: Retinal detachments in Patients with Uveitis (2017)